Key Points
-
Patient referral to specialist palliative care is associated with improved quality of life, symptom control, patient and caregiver satisfaction, illness understanding, end-of-life care, costs of care, and, potentially, survival
-
Oncologists and general practitioners have an important role in the delivery of primary palliative care, and in facilitating timely referral of patients to specialist palliative-care teams
-
The integration of oncological and palliative care needs to be tailored to the demands of the individual health-care system and hospital setting, according to the resources available locally
-
Outpatient palliative-care clinics are a hallmark of integration, providing patients with access to specialist palliative care early in the disease trajectory, and can accommodate multiple repeat visits over time
-
Routine symptom screening with automatic referral criteria, combined (multidisciplinary) patient-care rounds, renaming palliative care to 'supportive care', and embedded oncology–palliative-care clinics represent potential strategies to encourage integration of care
-
Education initiatives include a mandatory palliative-care rotation for oncology fellows, combined palliative care and oncology educational activities for trainees, and continuing medical education in palliative care for practicing oncologists
Abstract
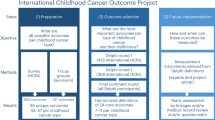
Over the past five decades, palliative care has evolved from serving patients at the end of life into a highly specialized discipline focused on delivering supportive care to patients with life-limiting illnesses throughout the disease trajectory. A growing body of evidence is now available to inform the key domains in the practice of palliative care, including symptom management, psychosocial care, communication, decision-making, and end-of-life care. Findings from multiple studies indicate that integrating palliative care early in the disease trajectory can result in improvements in quality of life, symptom control, patient and caregiver satisfaction, illness understanding, quality of end-of-life care, survival, and costs of care. In this narrative Review, we discuss various strategies to integrate oncology and palliative care by optimizing clinical infrastructures, processes, education, and research. The goal of integration is to maximize patient access to palliative care and, ultimately, to improve patient outcomes. We provide a conceptual model for the integration of supportive and/or palliative care with primary and oncological care. We also discuss how health-care systems and institutions need to tailor integration based on their resources, size, and the level of primary palliative care available.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Saunders, C. in The Management of Terminal Malignant Disease (eds Saunders, C. & Sykes, N.) 1–14 (Hodder and Stoughton, 1993).
Mount, B. M. The problem of caring for the dying in a general hospital; the palliative care unit as a possible solution. Can. Med. Assoc. J. 115, 119–121 (1976).
Hui, D. Definition of supportive care: does the semantic matter? Curr. Opin. Oncol. 26, 372–379 (2014).
Hui, D. et al. Concepts and definitions for “supportive care,” “best supportive care,” “palliative care,” and “hospice care” in the published literature, dictionaries, and textbooks. Support. Care Cancer 21, 659–685 (2013).
Lynch, T., Connor, S. & Clark, D. Mapping levels of palliative care development: a global update. J. Pain Symptom Manage. 45, 1094–1106 (2013).
Pastrana, T., Eisenchlas, J., Centeno, C. & De Lima, L. Status of palliative care in Latin America: looking through the Latin America Atlas of Palliative Care. Curr. Opin. Support. Palliat. Care 7, 411–416 (2013).
Centeno, C., Lynch, T., Donea, O., Rocafort, J. & Clark, D. EAPC Atlas of Palliative Care in Europe 2013 — Full Edition (European Association for Palliative Care, 2013).
Hui, D. et al. Availability and integration of palliative care at US cancer centers. JAMA 303, 1054–1061 (2010).
Hearn, J. & Higginson, I. J. Do specialist palliative care teams improve outcomes for cancer patients? A systematic literature review. Palliat. Med. 12, 317–332 (1998).
Higginson, I. J. et al. Do hospital-based palliative teams improve care for patients or families at the end of life? J. Pain Symptom Manage. 23, 96–106 (2002).
Zimmermann, C., Riechelmann, R., Krzyzanowska, M., Rodin, G. & Tannock, I. Effectiveness of specialized palliative care: a systematic review. JAMA 299, 1698–1709 (2008).
Hui, D. et al. Integration of oncology and palliative care: a systematic review. Oncologist 20, 77–83 (2015).
Temel, J. S. et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J. Clin. Oncol. 29, 2319–2326 (2011).
Temel, J. S. et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N. Engl. J. Med. 363, 733–742 (2010).
Zimmermann, C. et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 383, 1721–1730 (2014).
Bakitas, M. et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 302, 741–749 (2009).
Bakitas, M. et al. Early versus delayed initiation of concurrent palliative oncology care: patient outcomes in the ENABLE III randomized controlled trial. J. Clin. Oncol. 33, 1438–1445 (2015).
Hui, D. et al. Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer 120, 1743–1749 (2014).
Higginson, I. J. et al. Is there evidence that palliative care teams alter end-of-life experiences of patients and their caregivers? J. Pain Symptom Manage. 25, 150–168 (2003).
Higginson, I. J. et al. An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: a randomised controlled trial. Lancet Respir. Med. 2, 979–987 (2014).
Dudgeon, D. J. et al. Palliative Care Integration Project (PCIP) quality improvement strategy evaluation. J. Pain Symptom Manage. 35, 573–582 (2008).
Wright, A. A. et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300, 1665–1673 (2008).
Mack, J. W., Weeks, J. C., Wright, A. A., Block, S. D. & Prigerson, H. G. End-of-life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. J. Clin. Oncol. 28, 1203–1208 (2010).
Morrison, R. S. et al. Cost savings associated with US hospital palliative care consultation programs. Arch. Intern. Med. 168, 1783–1790 (2008).
Dyar, S., Lesperance, M., Shannon, R., Sloan, J. & Colon-Otero, G. A nurse practitioner directed intervention improves the quality of life of patients with metastatic cancer: results of a randomized pilot study. J. Palliat. Med. 15, 890–895 (2012).
Prince-Paul, M., Burant, C. J., Saltzman, J. N., Teston, L. J. & Matthews, C. R. The effects of integrating an advanced practice palliative care nurse in a community oncology center: a pilot study. J. Support. Oncol. 8, 21–27 (2010).
Payne, R. The integration of palliative care and oncology: the evidence. Oncology (Williston Park) 25, 1266 (2011).
Rangachari, D. & Smith, T. J. Integrating palliative care in oncology: The oncologist as a primary palliative care provider. Cancer J. 19, 373–378 (2013).
MacKenzie, M. A. The interface of palliative care, oncology and family practice: a view from a family practitioner. Can. Med. Assoc. J. 158, 1705–1707 (1998).
Hui, D. et al. Access to palliative care among patients treated at a comprehensive cancer center. Oncologist 17, 1574–1580 (2012).
Beccaro, M., Costantini, M., Merlo, D. F. & Group, I. S. Inequity in the provision of and access to palliative care for cancer patients. Results from the Italian survey of the dying of cancer (ISDOC). BMC Public Health 7, 66 (2007).
Morita, T., Miyashita, M., Tsuneto, S., Sato, K. & Shima, Y. Late referrals to palliative care units in Japan: nationwide follow-up survey and effects of palliative care team involvement after the Cancer Control Act. J. Pain Symptom Manage. 38, 191–196 (2009).
Schenker, Y. et al. Oncologist factors that influence referrals to subspecialty palliative care clinics. J. Oncol. Pract. 10, e37–e44 (2013).
Davis, M. P., Bruera, E. & Morganstern, D. Early integration of palliative and supportive care in the cancer continuum: challenges and opportunities. Am. Soc. Clin. Oncol. Educ. Book 2013, 144–150 (2013).
Rodriguez, K. L., Barnato, A. E. & Arnold, R. M. Perceptions and utilization of palliative care services in acute care hospitals. J. Palliat. Med. 10, 99–110 (2007).
Bruera, E. & Hui, D. Integrating supportive and palliative care in the trajectory of cancer: establishing goals and models of care. J. Clin. Oncol. 28, 4013–4017 (2010).
Tanco, K. et al. Patient perception of physician compassion after a more optimistic vs a less optimistic message: a randomized clinical trial. JAMA Oncol. 1, 176–183 (2015).
Dow, L. A. et al. Paradoxes in advance care planning: the complex relationship of oncology patients, their physicians, and advance medical directives. J. Clin. Oncol. 28, 299–304 (2010).
Lamont, E. B. & Siegler, M. Paradoxes in cancer patients' advance care planning. J. Palliat. Med. 3, 27–35 (2000).
Davis, M. P., Strasser, F. & Cherny, N. How well is palliative care integrated into cancer care? A MASCC, ESMO, and EAPC Project. Support. Care Cancer 23, 2677–2685 (2015).
Davis, M. P., Strasser, F., Cherny, N. & Levan, N. MASCC/ESMO/EAPC survey of palliative programs. Support. Care Cancer 23, 1951–1968 (2014).
Kloke, M. & Scheidt, H. Pain and symptom control for cancer patients at the University Hospital in Essen: integration of specialists' knowledge into routine work. Support. Care Cancer 4, 404–407 (1996).
Strasser, F. et al. Impact of a half-day multidisciplinary symptom control and palliative care outpatient clinic in a comprehensive cancer center on recommendations, symptom intensity, and patient satisfaction: a retrospective descriptive study. J. Pain Symptom Manage. 27, 481–491 (2004).
Follwell, M. et al. Phase II study of an outpatient palliative care intervention in patients with metastatic cancer. J. Clin. Oncol. 27, 206–213 (2009).
Bruera, E. & Hui, D. Conceptual models for integrating palliative care at cancer centers. J. Palliat. Med. 15, 1261–1269 (2012).
Gaertner, J. et al. Implementing WHO recommendations for palliative care into routine lung cancer therapy: a feasibility project. J. Palliat. Med. 13, 727–732 (2010).
Hydeman, J. Improving the integration of palliative care in a comprehensive oncology center: increasing primary care referrals to palliative care. Omega (Westport) 67, 127–134 (2013).
Shamieh, O. & Hui, D. A comprehensive palliative care program at a tertiary cancer center in Jordan. Am. J. Hosp. Palliat. Care 32, 238–242 (2015).
Smith, A. K. et al. The diverse landscape of palliative care clinics. J. Palliat. Med. 16, 661–668 (2013).
Yennurajalingam, S. et al. Clinical response to an outpatient palliative care consultation in patients with advanced cancer and cancer pain. J. Pain Symptom Manage. 44, 340–350 (2012).
Yoong, J. et al. Early palliative care in advanced lung cancer: a qualitative study. JAMA Intern. Med. 173, 283–290 (2013).
Kang, J. H., Kwon, J. H., Hui, D., Yennurajalingam, S. & Bruera, E. Changes in symptom intensity among cancer patients receiving outpatient palliative care. J. Pain Symptom Manage. 46, 652–660 (2013).
Hui, D. et al. Minimal clinically important differences in the Edmonton Symptom Assessment Scale in cancer patients: a prospective study. Cancer 121, 3027–3035 (2015).
Arthur, J. & Bruera, E. in Palliative Care in Oncology (eds Alt-Epping, B. & Nauck, F.) 1–11 (Springer, 2015).
Muir, J. C. et al. Integrating palliative care into the outpatient, private practice oncology setting. J. Pain Symptom Manage. 40, 126–135 (2010).
Johnston, B., Buchanan, D., Papadopoulou, C., Sandeman, G. & Lord, H. Integrating palliative care in lung cancer: an early feasibility study. Int. J. Palliat. Nurs. 19, 433–437 (2013).
Okuyama, T. et al. Oncologists' recognition of supportive care needs and symptoms of their patients in a breast cancer outpatient consultation. Jpn J. Clin. Oncol. 41, 1251–1258 (2011).
Lee, S. J., Katona, L. J., De Bono, S. E. & Lewis, K. L. Routine screening for psychological distress on an Australian inpatient haematology and oncology ward: impact on use of psychosocial services. Med. J. Aust. 193, S74–S78 (2010).
Wagner, L. I. et al. Bringing PROMIS to practice: brief and precise symptom screening in ambulatory cancer care. Cancer 121, 927–934 (2015).
Carlson, L. E., Groff, S. L., Maciejewski, O. & Bultz, B. D. Screening for distress in lung and breast cancer outpatients: a randomized controlled trial. J. Clin. Oncol. 28, 4884–4891 (2010).
Palmer, S. C., van Scheppingen, C. & Coyne, J. C. Clinical trial did not demonstrate benefits of screening patients with cancer for distress. J. Clin. Oncol. 29, e277–e278 (2011).
Khatcheressian, J. et al. Improving palliative and supportive care in cancer patients. Oncology (Williston Park) 19, 1365–1376 (2005).
Gaertner, J. et al. Specifying WHO recommendation: moving toward disease-specific guidelines. J. Palliat. Med. 13, 1273–1276 (2010).
Weissman, D. E. & Meier, D. E. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J. Palliat. Med. 14, 17–23 (2011).
Center to Advance Palliative Care. Your hub for palliative care innovation, development and growth [online], (2015).
Adelson, K., Paris, J., Smith, C. B., Horton, J. & Morrison, S. R. Standardized criteria for required palliative care consultation on the solid tumor oncology service [abstract]. J. Clin. Oncol. 31 (Suppl. 31), a37 (2013).
Levy, M. H. et al. Palliative care. J. Natl Compr. Canc. Netw. 10, 1284–1309 (2012).
Glare, P. et al. Study using the NCCN guidelines for palliative care to screen patients for palliative care needs and referral to palliative care specialists. J. Natl Compr. Canc. Netw. 11, 1087–1096 (2013).
Glare, P. A., Semple, D., Stabler, S. M. & Saltz, L. B. Palliative care in the outpatient oncology setting: evaluation of a practical set of referral criteria. J. Oncol. Pract. 7, 366–370 (2011).
Glare, P. A. & Chow, K. Validation of a simple screening tool for identifying unmet palliative care needs in patients with cancer. J. Oncol. Pract. 11, e81–e86 (2015).
Cherny, N. I. Stigma associated with “palliative care”: getting around it or getting over it. Cancer 115, 1808–1812 (2009).
Fadul, N. et al. Supportive versus palliative care: what's in a name?: a survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer 115, 2013–2021 (2009).
Dalal, S. et al. Association between a name change from palliative to supportive care and the timing of patient referrals at a comprehensive cancer center. Oncologist 16, 105–111 (2011).
Hui, D. et al. Attitudes and beliefs toward supportive and palliative care referral among hematologic and solid tumor oncology specialists. Oncologist http://dx.doi.org/10.1634/theoncologist.2015-0240 (2015).
Wentlandt, K. et al. Referral practices of oncologists to specialized palliative care. J. Clin. Oncol. 30, 4380–4386 (2012).
Maciasz, R. M. et al. Does it matter what you call it? A randomized trial of language used to describe palliative care services. Support. Care Cancer 21, 3411–3419 (2013).
Aapro, M. S. Supportive care and palliative care: a time for unity in diversity. Ann. Oncol. 23, 1932–1934 (2012).
Vergo, M. T. & Cullinan, A. M. Joining together to improve outcomes: integrating specialty palliative care into the care of patients with cancer. J. Natl Compr. Canc. Netw. 11, S38–S46 (2013).
Colombet, I. et al. Effect of integrated palliative care on the quality of end-of-life care: retrospective analysis of 521 cancer patients. BMJ Support. Palliat. Care 2, 239–247 (2012).
Porzio, G. et al. Integrating oncology and palliative home care in Italy: the experience of the “L'Aquila per la Vita” Home Care Unit. Tumori 99, 225–228 (2013).
Abrahm, J. L. Integrating palliative care into comprehensive cancer care. J. Natl Compr. Canc. Netw. 10, 1192–1198 (2012).
Hui, D. et al. Indicators of integration of oncology and palliative care programs: an international consensus. Ann. Oncol. 26, 1953–1959 (2015).
Cherny, N. I., Catane, R. ; European Society of Medical Oncology Taskforce on Palliative & Supportive Care. Attitudes of medical oncologists toward palliative care for patients with advanced and incurable cancer: report on a survery by the European Society of Medical Oncology Taskforce on Palliative and Supportive Care. Cancer 98, 2502–2510 (2003).
Ferris, F. D. et al. Palliative cancer care a decade later: accomplishments, the need, next steps. J. Clin. Oncol. 27, 3052–3058 (2009).
Education in Palliative and End-of-life Care. Welcome to EPEC [online], (2015).
Robinson, K. et al. Assessment of the Education for Physicians on End-of-Life Care (EPEC) Project. J. Palliat. Med. 7, 637–645 (2004).
Cole, B. E. An EPEC weekend. Am. J. Hosp. Palliat. Care 16, 467–470 (1999).
VanGeest, J. B. Process evaluation of an educational intervention to improve end-of-life care: the Education for Physicians on End-of-Life Care (EPEC) program. Am. J. Hosp. Palliat. Care 18, 233–238 (2001).
American Association of Colleges of Nursing. ELNEC Fact Sheet [online], (2015).
Coyne, P. et al. Oncology End-of-Life Nursing Education Consortium training program: improving palliative care in cancer. Oncol. Nurs. Forum 34, 801–807 (2007).
Ferrell, B., Malloy, P. & Virani, R. The end of life nursing education nursing consortium project. Ann. Palliat. Med. 4, 61–69 (2015).
Tsuneto, S. Past, present, and future of palliative care in Japan. Jpn J. Clin. Oncol. 43, 17–21 (2013).
Japanese Society for Palliative Medicine. Palliative care Emphasis program on symptom management and Assessment for Continuous medical Education (PEACE) [online], (2015).
Yamamoto, R. et al. Outcome evaluation of the Palliative care Emphasis program on symptom management and Assessment for Continuous Medical Education: nationwide physician education project for primary palliative care in Japan. J. Palliat. Med. 18, 45–49 (2015).
Pallium Canada. LEAP–Learning Essential Approaches to Palliative and End-of-Life Care Courseware [online], (2015).
ASCO Institute for Quality. ASCO Virtual Learning Collaborative [online], (2015).
Pallium Canada. LEAP Mini Onco [online], (2015)
Conquer Cancer Foundation of the American Society of Clinical Oncology. Palliative Care in Oncology Symposium [online], (2015).
Multinational Association of Supportive Care in Cancer. Supportive Care Makes Excellent Cancer Care Possible [online], (2015).
The University of Texas MD Anderson Cancer Center. Updates in Hospice and Palliative Medicine and Intensive Board Review [online], (2015).
Harvard Medical School. Center for Palliative Care [online], (2015).
International Association for Hospice and Palliative Care. Directory of Educational Programs in Palliative Care [online], (2015).
Morita, T. et al. Effects of a programme of interventions on regional comprehensive palliative care for patients with cancer: a mixed-methods study. Lancet Oncol. 14, 638–646 (2013).
Jost, L. & Roila, F. Management of cancer pain: ESMO clinical recommendations. Ann. Oncol. 20 (Suppl. 4), 170–173 (2009).
Cherny, N. I. ESMO Clinical Practice Guidelines for the management of refractory symptoms at the end of life and the use of palliative sedation. Ann. Oncol. 25 (Suppl. 3), iii143–iii152 (2014).
Levy, M. H. et al. Palliative care, Version 1.2014. Featured updates to the NCCN Guidelines. J. Natl Compr. Canc. Netw. 12, 1379–1388 (2014).
Schrijvers, D. & Cherny, N. I. ESMO Clinical Practice Guidelines on palliative care: advanced care planning. Ann. Oncol. 25 (Suppl. 3), iii138–iii142 (2014).
Fabrice, A. et al. ESMO/ASCO Recommendations for a Global Curriculum in Medical Oncology: 2010 Update [online], (2010).
Hansen, H. H. et al. Recommendations for a global core curriculum in medical oncology. J. Clin. Oncol. 22, 4616–4625 (2004).
Buss, M. K. et al. Hematology/oncology fellows' training in palliative care: results of a national survey. Cancer 117, 4304–4311 (2011).
Legrand, S. B. & Heintz, J. B. Palliative medicine fellowship: a study of resident choices. J. Pain Symptom Manage. 43, 558–568 (2012).
von Gunten, C. F. & Lupu, D. Development of a medical subspecialty in palliative medicine: progress report. J. Palliat. Med. 7, 209–219 (2004).
von Gunten, C. F., Sloan, P. A., Portenoy, R. K. & Schonwetter, R. S. Physician board certification in hospice and palliative medicine. J. Palliat. Med. 3, 441–447 (2000).
Yamaguchi, T. et al. Palliative care development in the Asia-Pacific region: an international survey from the Asia Pacific Hospice Palliative Care Network (APHN). BMJ Support. Palliat. Care http://dx.doi.org/10.1136/bmjspcare-2013-000588 (2014).
Hui, D., Finlay, E., Buss, M. K., Prommer, E. & Bruera, E. Palliative oncologists: specialists in the science and art of patient care. J. Clin. Oncol. 33, 2314–2317 (2015).
Hui, D. et al. Quantity, design, and scope of the palliative oncology literature. Oncologist 16, 694–703 (2011).
Hui, D., Arthur, J., Dalal, S. & Bruera, E. Quality of the supportive and palliative oncology literature: a focused analysis on randomized controlled trials. Support. Care Cancer 20, 1779–1785 (2012).
Hui, D., Reddy, A., Parsons, H. A. & Bruera, E. Reporting of Funding Sources and Conflict of Interest in the Supportive and Palliative Oncology Literature. J. Pain Symptom Manage. 44, 421–430 (2012).
Curtis, J. R. & Morrison, R. S. The future of funding for palliative care research: suggestions for our field. J. Palliat. Med. 12, 26–28 (2009).
Page, B. What is Supportive Care? Can. Oncol. Nurs. J. 4, 62–63 (1994).
Casarett, D., Johnson, M., Smith, D. & Richardson, D. The optimal delivery of palliative care: a national comparison of the outcomes of consultation teams vs inpatient units. Arch. Intern. Med. 171, 649–655 (2011).
Acknowledgements
The work of D.H. is supported in part by a Mentored Research Scholar Grant in Applied and Clinical Research (MRSG-14-148-01–CCE) from the American Cancer Society, and a National Institutes of Health grant (R21CA186000-01A1). The work of E.B. is supported in part by National Institutes of Health grants R01NR010162-01A1, R01CA122292-01, and R01CA124481-01.
Author information
Authors and Affiliations
Contributions
Both authors researched data for the article, contributed to discussion of content, and wrote and reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Hui, D., Bruera, E. Integrating palliative care into the trajectory of cancer care. Nat Rev Clin Oncol 13, 159–171 (2016). https://doi.org/10.1038/nrclinonc.2015.201
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2015.201
This article is cited by
-
The impact of early palliative care on the quality of life of patients with advanced pancreatic cancer: The IMPERATIVE case-crossover study
Supportive Care in Cancer (2023)
-
Development of the palliative care referral system: proposal of a tool for the referral of cancer patients to specialized palliative care
BMC Palliative Care (2022)
-
Von der „frühen“ zur „zeitgerechten“ Integration der Palliativversorgung in die Behandlung onkologischer Patient:innen
Die Onkologie (2022)
-
Risk stratification for clinical severity of pulmonary embolism in patients with cancer: a narrative review and MASCC clinical guidance for daily care
Supportive Care in Cancer (2022)
-
Palliative, palliative or palliative?
Critical Care (2021)