Abstract
Background
End-of-life decisions are frequently made by patients’ surrogates. Race and ethnicity may affect such decision making. Few studies have described how different racial/ethnic groups experience end-of-life surrogate decision making.
Objectives
To describe the self-reported experience the self-reported experience of African-American, Caucasian, and Hispanic surrogate decision makers of seriously ill patients and to examine the relationship of race, ethnicity, and culture to that experience.
Design
Purposive sample to include racial/ethnic minorities in a qualitative study using focus group interviews.
Participants
The participants of the study were 44 experienced, mostly female, surrogate decision makers for older veterans.
Approach
Transcripts were qualitatively analyzed to identify major themes, with particular attention to themes that might be unique to each of the three groups.
Results
The experience of burden of end-of-life decision making was similar in all three groups. This burden in its medical, personal, and familial dimensions is compounded by uncertainty about prognosis and the patient’s preferences. Racial/ethnic variations of responses to this burden concerned the physician–family relationship, religion and faith, and past experiences with race/ethnicity concordant versus non-concordant physicians.
Conclusions
Regardless of race/ethnicity, surrogates for seriously ill patients appeared to experience increased significant, multidimensional burdens of decision making under conditions of uncertainty about a patient’s preferences. This aspect of the burden of surrogate decision making may not be fully appreciated by physicians. Physicians should identify and be especially attentive to strategies used by surrogates, which may vary by race/ethnicity, to reduce the uncertainty about a patient’s preferences and thus the burden of surrogate decision making to assist them in this difficult process.
Similar content being viewed by others
INTRODUCTION
Given the increasing incidence with aging of cognitive disorders affecting the decision-making capacity of seriously ill elderly patients, surrogate decision making for such patients will become more common. Decision-making for others is challenging and compounded by the low rates of completing advance directives.1 Physicians need to understand how surrogates experience the process of end-of-life decision making to assist them in this difficult task. In addition, with the increasing racial and ethnic diversity among the elderly population, physicians need to improve their skills of culturally sensitive end-of-life decision making with surrogates.
Race and ethnicity affect end-of-life treatment preferences. Evidence indicates African-American patients prefer more aggressive treatment than Caucasians, as demonstrated by their lower use of do-not-resuscitate (DNR) orders, higher preference for cardiopulmonary resuscitation (CPR) and feeding tubes, and lower likelihood of withdrawal of life-sustaining therapy.2–17 Decisions regarding such care are often made by surrogates because patients are too ill to participate in the decision-making process. Nevertheless, few studies have focused on decision making by surrogates of seriously ill patients who actually played a major role in the decision-making process.18–21 Most studies addressing end-of-life decision making that included racially/ethnically diverse participants are either from the patients’ perspective or used convenience samples of older adults.2,10,22–26 Rare studies have considered the experience in terms of how race or ethnicity relates to surrogate decision making and then have focused on the African American perspective.7,27 Much less is known about the decision-making experiences of Hispanic surrogates, despite the fact that Hispanics represent the fastest growing minority group among older adults in the United States.28
The goals of this study were to describe self-reported experiences of surrogate end-of-life decision-making and to generate hypotheses about the relationship of race, ethnicity, and culture to that experience. This qualitative approach is open to the discovery of both commonalities and differences.
METHODS
Study Sample
After obtaining IRB approval, participants were recruited through the Michael E. DeBakey VA Medical Center (MEDVAMC) in Houston, Texas. We identified and recruited experienced surrogate decision makers for seriously ill patients, defining seriously ill similarly as in the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT; Table 1).29 Surrogates were identified via screening of the electronic medical records of patients who were either acutely ill or who had died within the last 3 months. For living patients, surrogates were included when patients were still hospitalized or had been discharged within the past 4 weeks. We chose this time frame to ensure that the decision-making process could still be recalled reliably. Surrogate status was based on emergency-contact information in the patient’s medical record followed by verbal confirmation from the surrogate. Surrogates received a postcard asking for participation and included a phone number to opt out. If they did not opt out, surrogates were called to explain the study and to obtain preliminary consent to participate. Race/ethnicity was determined by self-identification.
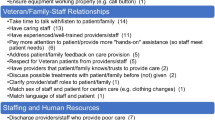
Figure 1 shows how the focus groups, each homogenous by race/ethnicity, were organized. Female trained moderators of the same race or ethnicity as the respective focus group conducted the groups.
Focus Group Procedures
Guiding questions were developed by the investigators after extensive literature review (Table 2). The moderators prompted participants to elaborate on responses. Comments and responses of other group members also served as prompts for obtaining additional information about participants’ experiences.30 After obtaining informed consent, focus groups, lasting 90 to 120 minutes, were conducted and audiotaped at MEDVAMC; then tapes were transcribed for qualitative analysis. For confidentiality, only codes, not names, were used in transcripts. Transcribers were not informed about race/ethnicity of participants.
ANALYSIS
We conducted inductive qualitative content analysis to identify ideas and concerns.31,32 Each investigator independently read transcripts, identified passages describing values or concerns, and assigned codes indicating emerging conceptual categories. We then compared our initial findings to identify and reconcile differences. Statements about values and concerns were coded and grouped into conceptual categories or themes using a consensus process among the investigators. Themes were reexamined for clarity and conciseness. We used a reiterative process of rereading and recoding passages, refining coding simultaneously, until final consensus was reached. We selected representative quotations from the transcripts illustrating the final categories and themes using ATLAS.ti 5.0.66 (Scientific Software Development GmbH, Berlin) to create a coded electronic data set.
RESULTS
We screened 367 patients, identified 172 (46.9%) eligible patients, and were able to identify surrogates for 83 of these patients. Of these, 44 (53.0%) agreed to participate in 1 of 8 focus groups (Fig. 1). The mean age of participants was 57.8 years (Table 3). About half of surrogates were patients’ spouses, and a quarter consisted of patients’ daughters. All but one were women.
The following paragraphs describe common themes that emerged across groups (Table 4). Next, themes more evident in particular racial and ethnic groups are presented.
Burden of Decision-making
The dominant theme in all groups was the tremendous burden of medical decision-making. Surrogates reported feeling enormous stress when having to make a decision for a patient for whom the clinical outcome was uncertain and no reliable account of the patient’s values, beliefs, or preferences was available. Having to decide under time pressure added distress. In addition, some surrogates voiced feeling a lack of control about their power to stop certain treatments once started. Obvious burdens on the patient, e.g., difficult-to-control pain or visible bloating from fluid overload, reduced the burden of decision making and led to less inclination for aggressive treatment. Surrogates stated that having discussions with patients about end-of-life treatment preferences was difficult, unless patient initiated.
Reported burden appeared to be keenly experienced on a personal level. Deciding upon a particular course of medical treatment for a loved one meant acknowledging the potential loss of that person’s life, and surrogates felt responsible for their decision. Surrogates felt conflicted about implementing a patient’s choice to decline life-prolonging therapy for fear of losing the patient: “You’re taking this person’s life in your hands,” one Hispanic surrogate remarked, “so you ask questions.” A Caucasian surrogate said, “It’s a lot like being on a jury in a murder trial, and you’ve got to determine whether this guy’s going to go sit on death row.... it’s a horrible burden upon the juror.”
Many surrogates reported feeling very alone in having to make major decisions without much assistance. They stated feeling very torn when other family members wanted to pursue treatment other than that elected by the surrogate and worried about being blamed by other relatives for making “wrong” treatment decisions. They also remarked feeling responsible for other decisions that had consequences for family members. For example, while not knowing when “the end” was near, they nonetheless believed they had to decide when or when not to call family members to the hospital to pay their last respects. This put stress on surrogates by forcing judgments about making other family members miss work and potentially lose a job, weighed against not being able to say “good-bye” if not called.
Factors that Increased the Burden of End-of-life Decision Making
Problems with Doctor–Patient Communication
All groups expressed the need for more jargon-free, understandable information regarding the patient’s health status and expected outcomes. All groups agreed that most doctors did not take enough time to explain things; physicians who did were most valued. Participants wished to receive detailed information about all aspects of care, including prognosis and chances of success in achieving desired outcomes associated with different interventions.
Surrogates voiced frustration about inability to get doctors to talk to them. Some reported perceiving doctors as “not forthcoming” about the patient’s medical care. When surrogates received answers, they often felt those were “not satisfactory,” although some admitted it might have been because “doctors don’t have all the answers.” Others reported that “doctors only call you for bad news,” “too late,” and “you feel unprepared”. All groups complained about difficulties in communicating with physicians.
Organizational Factors
All groups expressed dissatisfaction with lack of continuity of care resulting from rotations at a teaching hospital. Many surrogates stated that just when they had created rapport with some physicians, they were replaced by the next team. Being in a teaching hospital compounded a feeling of mistrust in some. One African-American surrogate remarked, “All of the interns come through and play with you.... It is that bad, because here—right here—they walk in with a crew. There’s four or five students—interns—with one overseer. And he stands back and he’ll talk about what has happened and let you guess upon what’s going on. And then they go in the hall and huddle to write notes on what our thinks are.”
Sometimes restrictive visiting hours created a barrier to surrogates seeking information. Surrogates believed doctors were “always rushed”, and some expressed suspecting that doctors “might not be allowed to say certain things”, creating distrust and the need to corroborate information they received, e.g., through internet resources.
Chances of Achieving an Acceptable Functional Outcome at an Acceptable Cost
Major goals across all racial/ethnic groups were to make the patient comfortable, pain-free, and not “to die as a vegetable or hooked up to machines for a long period of time”. Most surrogates were willing to pursue aggressive treatment only if chances for either some functional independence or some cognitive capacities were fairly high, although many African-American surrogates were willing to accept smaller chances of success. Uncertainty about the chances of such success increased the decision-making burden. Some surrogates reported loved ones being concerned about the financial costs of care, adding to the burden. One African-American surrogate explained, “He says, “I don’t want to be a burden. We’re not rich people, and it doesn’t make sense to put all your money on me, trying to keep me alive and I’m not really there.” A Caucasian surrogate voiced similar concerns: “My mother used to always tell me, ‘Don’t keep me on a machine that’s going to cost a fortune to just keep me there in a shell.”
Factors that Decreased the Burden of End-of-life Decision-making
Decision-‘Making’ Versus ‘Reporting’ a Decision
Some surrogates reported not making a decision de novo for the patient, i.e., identifying alternatives and weighing them against each other. Instead, they described their experience as simply reporting or executing decisions previously made by the patient. Because this was not perceived as having to ‘make’ a decision, this was experienced as much less burdensome: “I’m glad I was not put in the position that I had to make the decision for him.”[…] “He was coherent enough at that point in time to make the decision and me honor it.” An African-American surrogate said, “If anything happens, I know what he has said, and I just make sure that they do that. That’s all. No decision has to be made... that’s it.” An African-American surrogate said, “It was all written out, you know, like planned. And, we was like the overseers, you know, to see that it was done.” One summed it up by saying, “I’m more or less an enforcer.”
Trial of Intervention
Surrogates across all racial and ethnic groups brought up without prompting the concept of time-limited trials of interventions as a means to decrease the pressure of deciding. “Like she said, maybe the ventilator helped him for a limited amount of time which is fine. It took them over the hump, you know, […] that’s if you know that they’re going to possibly be able to get over that hump, but if they’re at the very end of their life and you already know that you’re not going to want to be on a ventilator.”
“Just work with me here and I work with you and we’ll just go—we’ll take each day at a time and see what happens […]—how he reacts or how it works for him” (Hispanic surrogates). However, some surrogates expressed feeling a lack of control and were confused about their right to stop interventions once they were started.
Faith, Religion, and Spirituality
Some surrogates in each of the groups expressed confidence that God is in charge of when someone dies and that God will take care of everyone. Surrogates said this belief facilitated decision making because it implied that God would help them make the “right” decisions. “God has the last say. He’s going to take you anyway when He gets ready, but by all means you do what you supposed to do for me before I leave here” (African-American surrogate). Some members across all groups viewed doctors as “instruments” of God and expressed the belief that God “leads and directs” doctors.
Some surrogates also expressed their belief in miracles: One Hispanic surrogate said, “I very deeply believe, and I always ask God for help. And I believe in miracles.” Other surrogates defined miracles differently, or did not “expect” them but rather prayed for strength, both for the patient and themselves: “I believe in God,” one Hispanic surrogate said, “and I always pray, but I pray different. I pray for Him to give him [the patient] the strength.”
Social Support
Surrogates relied on family, friends, and church members to cope with the burden of decision making for critically ill patients. Almost all participants had such support networks in place. However, several participants stated that they would have appreciated enormously having had access to other members in their focus group at the time of their own decision making, to learn from experiences of surrogates in similar positions of decision making.
Race or Ethnicity and Decision-making Experiences Among Surrogates
The Physician–Family Relationship
Certain beliefs were expressed only by members of specific racial/ethnic groups or in a distinctive manner. Hispanic surrogates in particular stated that they wished that doctors would be more proactive in convincing patients to discuss their health with family: “Hispanic men,” one remarked, “they’re very, very big on not wanting their family to deal with [illness], so they don’t tell them how sick they are: ‘I had a doctor’s appointment. Everything went fine.’ they may have told them. You know, the doctor could have told them that same day, you know, ‘We give you a month,’ but they’re not going to tell the family. They’ll just hold it within themselves, and that’s not fair to the family and that’s not fair to the patient, you know.... I, I mean, this isn’t my first rodeo. This is my second, you know, with Hispanic men.”
Although all surrogates thought physician–patient communication could improve, Hispanic surrogates in particular expressed a high level of appreciation for physicians who took time to speak to the family as a group. They expressed desire for physicians to mediate between patients and themselves and confessed that “Hispanic men don’t ask doctors enough questions—the pride thing.” Thus, they reported preferring a more proactive role on the physician’s part to address end-of-life issues earlier and to have doctors “order” the patient to discuss such issues with his family. Finally, Hispanics expressed the most anxiety about other relatives blaming them for making “wrong” decisions for patients.
While all groups asked for better communication with doctors, African-American surrogates voiced that doctors should be more approachable, less “abrasive,” or “intimidating,” and more “sensitive;” nonetheless, they appreciated honesty. However, they noted that bad news should be delivered by “easing families into the bad news.”
Religion and Faith
Many Hispanics reported viewing suffering as a “test of faith.” Regarding the issue of how far to push end-of life interventions, Hispanics seemed more divided; not all reported feeling that relatives had to “keep going until [the patient] and God say ‘no more,’” a view most African Americans expressed.
Most African-American participants reported that “doing everything” was the “right” thing to do, but “the rest was up to God”. That God could do anything suggested a duty to do “everything” to prolong life. Suffering was again viewed as a test of faith and an opportunity for moral growth, knowing that God would not “put more on you than you can bear”. A few even saw disease and suffering as punishment: “you reap what you have sowed.” Some “decisions” may not have been experienced as true “decisions:” for some participants, there appeared to be no choice when one’s faith required one to “do everything.” African Americans said additionally that God is an “intervener” in the course of medical care. One said, “God is a healer and if it’s going to, if it’ll be healed or whatever, He’ll control it.”
Among Caucasian surrogates, faith and spirituality were also noted as being very important in decision making. However, discussions related to faith and spirituality were much briefer than in the other groups. Caucasians reported viewing God as the one who decides the outcome. However, in contrast to most African Americans, they did not seem to feel the need to “do everything” to prolong life: “I knew it was in His hands,” said one, “I didn’t have any control over it. I was just one of the play actors on the game board.” Another explained, “That’s when your faith comes in, because I felt like God’s in control now, I’m not, and the decision’s been made, and whatever’s going to happen is going to happen.” Caucasians did not address suffering beyond noting that some suffering may be worth it if the patient has a chance to get well.
Experience with Race/Ethnicity Concordant Versus Not-concordant Physicians
Most African-American and Hispanic surrogates reported having little or no experience with physicians of their own race/ethnicity, and they reported valuing physician competence and trust in the physician without regard to racial or ethnic physician–patient concordance. Our direct question about whether surrogates had ever felt treated differently by physicians of a different race/ethnicity did not yield direct answers. However, at least one surrogate reported receiving inferior treatment when she was a patient herself, which she attributed to race.
One of the African American surrogates reflected on the fact that things might have changed over time and that there were more options in selecting physicians now than previously. She stated, “We always have... from child on... had a favorite doctor, a favorite race of doctors, that we had more confidence in....But, now I think that it’s a mixed emotion, who we may have confidence in.”
DISCUSSION
Other studies have examined surrogate decision making.33–36 Unlike these, we examined the relationship of race and ethnicity on the experience of surrogate decision making and used a purposive sampling strategy to include equal numbers of African American, Caucasian, and Hispanic surrogates in separate focus groups led by race-concordant moderators. None of these previous studies used such a strategy or made the relationship of race/ethnicity on surrogate decision making their primary focus. A few other studies have focused on the decision-making experience of racially and ethnically diverse surrogates deciding for seriously ill patients, but rather addressed their treatment preferences7 or problems with health care provider communication.27
The dominant theme in our analysis is the tremendous burden of decision-making surrogates experienced that transcended race/ethnicity. Surrogates reported feeling burdened in their expected role in medical, personal, and family domains. In the medical domain, burden appeared to vary directly with uncertainty about outcome and patients’ preferences. In the personal domain, surrogates reported fearing the loss of a loved one and feeling the weight of responsibility for such an outcome. In the family domain, surrogates reported making decisions that both left them open to criticism from other relatives and affected other relatives’ lives. Burdens in these three domains can become synergistic, compounding the challenges of surrogate decision making. Responses to these burdens can vary by race and ethnicity, especially in the context of religious beliefs about God’s power and the limits of medicine.
Others have pointed out the burden of surrogate decision making.37,38 We go further and describe two apparent contributors to the creation of such burden, uncertainty of prognosis, and uncertainty about the patient’s wishes. Our data also suggest that the multifaceted burden of surrogate decision making is an insufficiently appreciated challenge to surrogates and their physicians. Physicians could make changes to assist surrogates in their decision making. Improved physician–surrogate communication, in particular, the longer time that physicians can spend with surrogates in family conferences,39 and changes in the organizational culture of health care institutions could alleviate some of these burdens. For example, for some surrogates, offering a trial of intervention might be a helpful and underutilized strategy for making the decision-making burden more manageable, but only if surrogates have a clear understanding that they can stop interventions once begun as some of our participants believed they lacked that authority. The American College of Critical Care recently issued guidelines to support the family in the intensive care unit40 suggesting staff training to recognize and respond to family members’ stress. Our study adds the important insight that staff should appreciate such stress may be owed to the uncertainty about prognosis and the patient’s wishes and that such burden of decision-making-induced stress may transcend ethnicity and culture.
Many of the study participants appeared to perceive that decision making using the substituted judgment standard was not making a decision at all, but merely reporting a decision already made by the patient. The surrogates were willing to fulfill the role of reporting a decision already made, because they were not responsible for making a decision that would result in (although not necessarily cause) the death of their loved one.
While our identified themes applied to all races/ethnicities, responses to burdens of decision-making varied by race and ethnicity. For example, African American surrogates emphasized faith and spirituality more than any other group as major resource upon which they relied. It is worth noting that the alternative of nonintervention is sometimes not experienced as a viable option. Therefore, the phrase “making a decision” does not capture the experience of surrogates in such situations as some surrogates noted they did not understand themselves to have a choice in the matter. Religiously or spiritually based requests to “do everything” in end-of-life treatment should be explored with surrogate decision makers with this aspect in mind and not be prejudged as “unreasonable”.41
LIMITATIONS
One limitation of this study is a limitation of all qualitative focus group research, related to number and composition of the focus groups. Conduct of the study in an academic setting might limit generalizability. Conducted in a VA medical center, the patient population was predominantly male. Therefore, most surrogates were women. However, even outside the VA, caregivers, who often act as surrogates, are usually female.42 Thus, our findings are likely generalizable to other groups of surrogates. Strengths of our study are that we directly obtained information from surrogates well familiar with end-of-life decision making and purposively included racial and ethnic minorities.
Although we cannot be confident that differences between groups were due to race/ethnicity rather than another characteristic that may have differed among groups, ours is the first study to explore how the decision-making process for invasive procedures at the end of life might vary among surrogates from three racial/ethnic groups.
We did not triangulate our findings or use key informants. However, investigators were racially diverse and from different backgrounds (medicine, social sciences, ethics), and each read transcripts individually before getting to consensus. Last, this was a retrospective study, and participants may have been seeking to avoid cognitive dissonance in their recall of events, i.e., not wanting to see themselves as having made a bad or inappropriate decision.
CONCLUSION
Our data suggest that burdens faced by surrogates for seriously ill patients are common across race and ethnicity. These burdens and variable responses to them may not be fully appreciated by physicians. Physicians should be aware that surrogates use a variety of resources to cope with this burden and welcome help from physicians, especially clear and sensitive communication of information about the patient’s condition and prognosis. Our subjects emphasized the importance of physicians being available when surrogates have questions or concerns and ensuring adequate time for subsequent communication. Physicians should identify and be especially attentive to strategies used by surrogates to reduce the burdens of surrogate decision making to assist them in this difficult process.
References
Stelter KL, Elliott BA, Bruno CA. Living will completion in older adults. Arch Intern Med. 1992;1525954–9.
Blackhall LJ, Frank G, Murphy ST, Michel V, Palmer JM, Azen SP. Ethnicity and attitudes towards life sustaining technology. Soc Sci Med. 1999;48:1779–89.
Borum ML, Lynn J, Zhong Z. The effects of patient race on outcomes in seriously ill patients in SUPPORT: an overview of economic impact, medical intervention, and end-of-life decisions. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000;48:S194–S198.
Caralis PV, Davis B, Wright K, Marcial E. The influence of ethnicity and race on attitudes toward advance directives, life-prolonging treatments, and euthanasia. J Clin Ethics. 1993;4:155–65.
Degenholtz HB, Arnold RA, Meisel A, Lave JR. Persistence of racial disparities in advance care plan documents among nursing home residents. J Am Geriatr Soc. 2002;50:378–81.
Garrett JM, Harris RP, Norburn JK, Patrick DL, Danis M. Life-sustaining treatments during terminal illness: who wants what? J Gen Intern Med. 1993;8:361–68.
Hopp FP, Duffy SA. Racial variations in end-of-life care. J Am Geriatr Soc. 2000;48:658–63.
Kwak J, Haley WE. Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist. 2005;45:634–41.
Lahn M, Friedman B, Bijur P, Haughey M, Gallagher EJ. Advance directives in skilled nursing facility residents transferred to emergency departments. Acad Emerg Med. 2001;8:1158–62.
McKinley ED, Garrett JM, Evans AT, Danis M. Differences in end-of-life decision making among black and white ambulatory cancer patients. J Gen Intern Med. 1996;11:651–56.
Phipps E, True G, Harris D, Chong U, Tester W, Chavin SI, et al. Approaching the end of life: attitudes, preferences, and behaviors of African-American and white patients and their family caregivers. J Clin Oncol. 2003;21:549–54.
Shepardson LB, Gordon HS, Ibrahim SA, Harper DL, Rosenthal GE. Racial variation in the use of do-not-resuscitate orders. J Gen Intern Med. 1999;14:15–20.
Shepardson LB, Youngner SJ, Speroff T, O’Brien RG, Smyth KA, Rosenthal GE. Variation in the use of do-not-resuscitate orders in patients with stroke. Arch Intern Med. 1997;157:1841–47.
Teno JM, Licks S, Lynn J, Wenger N, Connors AF Jr., Phillips RS, et al. Do advance directives provide instructions that direct care. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. J Am Geriatr Soc. 1997;45:508–12.
Wenger NS, Pearson ML, Desmond KA, Harrison E, Rubenstein LV, Rogers WH, et al. Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med. 1995;155:2056–62.
Gessert CE, Curry NM, Robinson A. Ethnicity and end-of-life care: the use of feeding tubes. Ethn Dis. 2001;11:97–106.
Degenholtz HB, Thomas SB, Miller MJ. Race and the intensive care unit: disparities and preferences for end-of-life care. Crit Care Med. 2003;31:S373–S378.
Vig EK, Taylor JS, Starks H, Hopley EK, Fryer-Edwards K. Beyond substituted judgment: how surrogates navigate end-of-life decision-making. J Am Geriatr Soc. 2006;54:1688–93.
Heyland DK, Cook DJ, Rocker GM, Dodek PM, Kutsogiannis DJ, Peters S, et al. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Med. 2003;29:75–82.
Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–82.
Klinkenberg M, Willems DL, Onwuteaka-Philipsen BD, Deeg DJ, van der WG. Preferences in end-of-life care of older persons: after-death interviews with proxy respondents. Soc Sci Med. 2004;59:2467–77.
Shrank WH, Kutner JS, Richardson T, Mularski RA, Fischer S, Kagawa-Singer M. Focus group findings about the influence of culture on communication preferences in end-of-life care. J Gen Intern Med. 2005;208703–9.
Perkins HS, Geppert CM, Gonzales A, Cortez JD, Hazuda HP. Cross-cultural similarities and differences in attitudes about advance care planning. J Gen Intern Med. 2002;17:48–57.
Born W, Greiner KA, Sylvia E, Butler J, Ahluwalia JS. Knowledge, attitudes, and beliefs about end-of-life care among inner-city African Americans and Latinos. J Palliat Med. 2004;7:247–56.
Duffy SA, Jackson FC, Schim SM, Ronis DL, Fowler KE. Racial/ethnic preferences, sex preferences, and perceived discrimination related to end-of-life care. J Am Geriatr Soc. 2006;54:150–157.
Waters CM. Understanding and supporting African Americans’ perspectives of end-of-life care planning and decision making. Qual Health Res. 2001;11:385–98.
Jenkins C, Lapelle N, Zapka JG, Kurent JE. End-of-life care and African Americans: voices from the community. J Palliat Med. 2005;8:585–92.
Older Americans 2004 - Key indicators of well-being. Federal Interagency Forum on Aging-Related Statistics. 2004. Washington DC, U.S. Government Printing Office.
Murphy DJ, Knaus WA, Lynn J. Study population in SUPPORT: patients (as defined by disease categories and mortality projections), surrogates, and physicians. J Clin Epidemiol. 43. 1990:Suppl11S–28S.
Lofland J, Lofland L. Analyzing Social Settings: A Guide to Qualitative Observation and Analysis. 3rd edAlbany, New York: Wadsworth Publishing; 1995.
Krueger RA. Analyzing and reporting focus group results. In: Morgan DL, Krueger RA, eds. The Focus Group Kit. Thousand Oaks, CA: Sage Publications; 1998.
Morgan DL. Focus Groups in Qualitative Research. Qualitative Research Methods Series, Vol 16. Newbury Park, CA: Sage Publications; 1988.
Jacob DA. Family members’ experiences with decision making for incompetent patients in the ICU: a qualitative study. Am J Crit Care. 1998;7130–6.
Chambers-Evans J, Carnevale FA. Dawning of awareness: the experience of surrogate decision making at the end of life. J Clin Ethics. 2005;16128–45.
Tilden VP, Tolle SW, Nelson CA, Fields J. Family decision-making to withdraw life-sustaining treatments from hospitalized patients. Nurs Research. 2001;502105–115.
Abbott KH, Sago JG, Breen CM, Abernethy AP, Tulsky JA. Families looking back: one year after discussion of withdrawal or withholding of life-sustaining support. Crit Care Med. 2001;291197–201.
Prendergast TJ, Puntillo KA. Withdrawal of life support: intensive caring at the end of life. JAMA. 2002 Dec 4;288212732–40.
Lautrette A, Ciroldi M, Ksibi H, Azoulay E. End-of-life family conferences: rooted in the evidence. Crit Care Med. 2006 Nov;3411 SupplS364–72.
Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007 Feb 1;3565469–78.
Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004–2005. Crit Care Med. 2007;35:605–622.
Lo B, Ruston D, Kates LW, Arnold RM, Cohen CB, Faber-Langendoen K, et al. Discussing religious and spiritual issues at the end of life: a practical guide for physicians. JAMA. 2002;287:749–54.
Wakabayashi C, Donato KM. Does caregiving increase poverty among women in later life. Evidence from the Health and Retirement survey. J Health Soc Behav. 2006;473258–74. (Sep).
Acknowledgment
All authors thank JoLynn Mikow and Donna Espadas for their support in conducting the focus groups. Dr. Braun and this project were supported by a VA HSR&D Research Career Development Award, RCD 02029 and by NIA-R03-AG 022 144-01. Results of this study were presented in part at the Annual Meeting of the American Geriatric Society in Orlando, FL, in May 2005.
Conflict of Interest
The principal investigator and all coauthors have no conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Braun, U.K., Beyth, R.J., Ford, M.E. et al. Voices of African American, Caucasian, and Hispanic Surrogates on the Burdens of End-of-Life Decision Making. J GEN INTERN MED 23, 267–274 (2008). https://doi.org/10.1007/s11606-007-0487-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0487-7