Abstract
Purpose
Advanced cancer care planning is encouraged to achieve individualized care. We hypothesized that in-advance end-of-life (EOL) discussions and establishment of do-not-resuscitate (DNR) status prior to the terminal admission would be associated with better quality of inpatient EOL care.
Methods
We conducted a post-mortality survey, utilizing the validated Toolkit of Instruments to Measure End-of-Life Care. Primary caregivers (PCGs) of the advanced cancer patients who died at our institution between January 2009 and December 2010 were contacted more than 3 months after the patients’ death. The endpoints included overall score for EOL care (0–10; 10 = best care), problem scores of six domains (0–1; 1 = worst problem), and score for supporting family’s self-efficacy (knowing what to expect/do during the dying process) (1–3; 3 = greatest support).
Results
Of 115 PCGs contacted, 50 agreed to participate (43.5 %). Patients with EOL discussions (n = 20), as compared to those without (n = 29), had higher rating of overall EOL care (9.7 vs. 8.7; p = 0.001): lower problem scores in “informing and promoting shared decision-making” (0.121 vs. 0.239; p = 0.007), “encouraging advanced care planning” (0.033 vs. 0.167; p = 0.010), “focusing on individual” (0.051 vs. 0.186; p = 0.014), “attending to emotional/spiritual needs of family” (0.117 vs. 0.333; p = 0.010), and “providing care coordination” (0.100 vs. 0.198; p = 0.032), and greater support for family’s self-efficacy (2.734 vs. 2.310; p < 0.001). No significant differences were found in these outcomes between patients with DNR (n = 19) and those with full code (n = 31) on admission.
Conclusion
Advanced cancer patients may receive higher quality of inpatient EOL care if they had in-advance EOL discussions.
Similar content being viewed by others
Introduction
As many as 40 % of advanced cancer patients die in hospitals in the USA [1]. However, post-mortality surveys with primary caregivers (PCGs) have demonstrated that patients who died in hospitals experienced poorer quality of end-of-life (EOL) care as compared to those who died under hospice service [2, 3]. Wright et al. have reported that more than 10 % of the advanced cancer patients received aggressive medical care such as ICU admission, ventilator use, resuscitation, chemotherapy, and feeding tube in the last week of life. They also demonstrated that such care was associated with worse patient quality of life (QOL) and that having EOL discussions with doctors in advance correlated with a lower rate of aggressive care [4]. This finding suggests that an early implementation of advanced care planning (ACP) may improve the quality of EOL in advanced cancer patients. Advanced directives are used to formalize ACP that includes preferences with regard to code status in addition to living will and medical power of attorney. A large retrospective study revealed that a majority of advanced cancer patients who died in hospital had their code status changed from full code to do-not-resuscitate (DNR) on the day of death [5]. This extremely late transition may indicate an inadequate preparation for EOL care by patients and their families as well as health care professionals (HCPs) including physicians and nurses, which may lead to suboptimal EOL care. Although initiation of EOL discussions and establishment of DNR status prior to a terminal admission may jointly promote ACP, their impact on the quality of inpatient EOL care has never been evaluated comprehensively.
While measurement of the quality of EOL care is essential to improve the process of care toward excellent QOL, interviewing vulnerable terminally ill patients is burdensome. Therefore, studies have been conducted with PCGs who know the most about the patients’ situation near their death [2, 3, 6–9]. The Toolkit of Instruments to Measure End-of-Life Care (TIME) is a valid and reliable after-death interview toolkit that was developed to measure quality of EOL care from the unique perspective of PCGs [2].
Our primary objective in this study was to determine if (1) the presence of EOL discussions with a primary oncologist or PCP prior to the terminal admission as recollected by the PCG and (2) early establishment of DNR status prior to or on presentation to the terminal admission were associated with a better overall rating scale for inpatient EOL care in the last week of life as measured by TIME. Our secondary objective was to determine if these two factors were associated with a better quality of care in the following seven different domains in the last week of life as measured by TIME: (1) physical comfort and emotional support, (2) inform and promote shared decision-making, (3) encourage advance care planning, (4) focus on individual, (5) attend to the emotional and spiritual needs of the family, (6) provide coordination of care, and (7) support the self-efficacy of the family (help the family prepare for the patient’s dying and EOL care).
Methods
Participants
We conducted a post-mortality survey study of bereaved PCGs of advanced cancer patients who died during admission to Fletcher Allen Health Care (FAHC), a tertiary hospital affiliated with the University of Vermont College of Medicine.
Cancer patients who died at FAHC from January 2009 to December 2010 were eligible if they (1) had distant metastases, locally advanced malignancy with severe medical comorbidities or treatment complications, acute leukemia or stage III/IV lymphoma, or refractory disease to first-line chemotherapy, or (2) declined cancer treatment. We excluded patients who were under 18 years of age or those who died as a result of trauma or suicide. Eligibility of participating PCGs included (1) listed as the next of kin in the electronic medical record of an eligible patient, (2) age 18 or older, (3) English speaking, (4) reported as one of the people most involved in the patient’s care during the last few weeks of life when asked directly by the interviewer, (5) willing to participate in an interview, and (6) able to be contacted more than 3 months following the patient’s death. We chose this 3-month cutoff to avoid contacting PCGs during a state of acute grief [10].
Patient- and disease-related data of the eligible patients and their PCGs’ contact information were obtained from hospital administrative database. Permission was obtained from treating physicians (either primary oncologists or PCPs) to send an invitation letter to the potential PCGs. In cases where the study investigators had a treating relationship with the patients and neither primary oncologists nor PCPs were available, a letter was sent directly to the bereaved PCGs. Bereaved PCGs were informed by mail of the study availability, and information was provided to them with a response letter and toll-free number to use in order to agree or decline participation. If the respondents replied that they were not PCGs, they were asked to indicate PCGs’ contact information. Then a new invitation letter was mailed to the newly designated PCGs. Those who did not decline participation were telephoned to request their participation in the study. After receiving permission from the PCGs, we obtained informed consent and proceeded with an interview over the phone or in person. The principal investigator (MM) and a trained research assistant (DE) served as interviewers. The investigators performed the human investigations after approval by the University Institutional Review Board and in accord with an assurance filed with and approved by the Department of Health and Human Services.
Survey tool
TIME is an after-death interview toolkit designed to aid hospital staff in assessing and improving quality of EOL care [2]. TIME has been validated in bereaved PCGs of patients who died in hospitals and serves as an ideal tool to identify areas of improvement toward excellent inpatient EOL care [2]. The instrument produces an overall rating scale for the quality of inpatient EOL care, ranging from 1 to 10 with a higher score indicating better quality. Next, for the first six domains, the questions are summarized as “problem scores” that range from 0 to 1 with a higher number signifying more opportunity to improve: (1) physical comfort and emotional support, (2) inform and promote shared decision-making, (3) encourage advance care planning, (4) focus on individual, (5) attend to the emotional and spiritual needs of the family, and (6) provide coordination of care. The original validation study stated that an overall mean problem score greater than 0.20 was indicative of an important opportunity to improve the quality of care [2]. With the “physical comfort and emotional support” domain, the binary nature of the response (either 0 = problem absent or 1 = problem present) allowed us to calculate proportion of patients who had unmet needs based on the problem scores. Lastly, in order to evaluate the degree of support for the self-efficacy of the family, key questions are summarized on a three-point scale ranging from 1 to 3 with a higher score indicating greater self-efficacy.
Our primary outcome measure was overall rating scale (0–10). The secondary outcome measures were problem scores of the aforementioned six domains (0–1) and the score for supporting the self-efficacy of the family (1–3).
In order to determine whether EOL discussions took place prior to the terminal admission, we asked PCGs the following question: “Before [his/her] last admission, had [he/she] and [his/her] doctor discussed any particular wishes [he/she] had about the care [he/she] would want to receive when [he/she] was dying, such as code status, living will, or medical power of attorney?” This question was modified from the one used in the previous study [4] so that specific contents of EOL discussions could be identified. If the answer was yes, then we asked about the contents (code status, living will, medical power of attorney, or other) and person with whom the patient had EOL discussions (primary oncologist, PCP, or other).
Statistical analysis
Two-sample t tests and Chi-square tests were used to compare mean summary scores for baseline characteristics and survey outcomes. Analyses of variance were used for adjustment of outcome analyses for baseline differences between each of the two sets of two groups (presence vs. absence of EOL discussions; DNR vs. full code on admission). For categorical values in “physical comfort and emotional support domain”, binary logit analyses were performed for covariate adjustments using baseline differences.
Results
One hundred and twenty-nine of 189 cancer patients who died at FAHC from January 2009 to December 2010 were eligible for our study (Fig. 1). Of 115 PCGs who were contacted, 50 agreed to participate (43.5 %). The mean duration between the death and interview was 307.2 days.
Table 1 shows the baseline characteristics of the deceased patients and bereaved PCGs. The two patient groups based on the presence or absence of EOL discussions prior to the terminal admission were well matched except for the age. Of the 20 patients who had EOL discussions with their primary oncologists or PCPs prior to the terminal admission, 15 (75 %), 13 (65 %), and 10 (50 %) discussed code status, living will, and medical power of attorney, respectively. Eight (40 %) patients discussed all the three contents. The other two groups based on code status on presentation to the terminal admission had several significant baseline differences (Table 1).
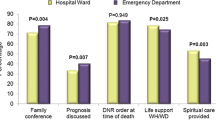
Table 2 summarizes the outcomes between groups with respect to the EOL discussions and code status. Analyses were adjusted for statistically significant baseline differences between the corresponding groups according to EOL discussion status and code status. Patients who had EOL discussions had significantly higher overall rating of inpatient cancer EOL care than those who did not have EOL discussions (9.7 vs. 8.6; p = 0.001). Among cancer patients with in-advance EOL discussions as compared to those without EOL discussions, a lower percentage of patients had unmet needs in all components of the “physical comfort and emotional support” domain, though these differences did not reach statistical significance. However, the former group had significantly lower problem scores in all the other domains than the latter. In particular, while no score exceeded 0.20 in the patients with EOL discussions, problem scores of “informing and promoting shared decision-making” (0.24) and “attending to the emotional and spiritual needs of the family” (0.33) were greater than this cutoff in those without EOL discussions, indicating a major opportunity to improve the quality of care for the latter group. Lastly, a self-efficacy scale demonstrated significantly higher score in the former group than in the latter (2.73 vs. 2.31; p < 0.001), indicating greater PCG preparation for patient’s EOL if the patients had in-advance EOL discussions.
To interpret these significant differences in more clinically meaningful way, we conducted ad hoc logistic regression analyses comparing percentages of participants who responded favorably to a selected representative question in each of the five problem domains and two representative questions in the self-efficacy domain (Table 3). The majority of patients who had in-advance EOL discussions were shown to have received significantly more patient-focused, family-centered EOL care in these items.
On the other hand, no statistically significant differences were observed in any of the outcomes between cancer patients with DNR and those with full code on admission (Table 2). In the domain of “attending to emotional and spiritual needs of family”, the patients with DNR tended to have less problems than those with full code (problem domain scores 0.218 vs. 0.263; adjusted p value = 0.071).
Discussion
The most unique and important finding in this pilot study was that having in-advance EOL discussions, rather than the decision about code status on presentation to the terminal admission, was the key predictor associated with higher quality of inpatient EOL care as perceived by bereaved PCGs. If the EOL discussions still resulted in a decision for full code on presentation and the patient died during the indicated admission, this may not lead to greater disappointment but rather to satisfaction that EOL issues had been discussed. This specific difference in implications of in-advance EOL discussions and code status on terminal admission has never been reported in previous studies [4, 11].
For some oncologists who view transition to EOL care as a “failure” to alter the disease course, initiating EOL discussions could be anxiety-provoking and presents some challenges in daily patient care [12, 13]. Our findings suggest that late transition to DNR, unlike failure to have in-advance EOL discussions, may not impair the quality of care during the terminal admission. This contrast highlights the fact that transition to EOL care is a process for both HCPs and patients/families. In the care of advanced cancer patients, transition to EOL is usually started by oncologists or PCPs who initiate conversations informing patients and their caregivers of the incurable nature of their disease and provide prognostic information. Treating physicians may also discuss care options and supporting resources available to them, and inquire about advanced directives. After such EOL discussions take place, patients and their caregivers can hold realistic conversations and consider their own needs, goals, wishes, and preferences purposefully [14]. Their decision-making can evolve over time, and they may or may not complete advanced directives. Decision of code status can be one of the end results of such a decision-making process.
Another key finding was that initiation of EOL discussions prior to the terminal admission was significantly associated with higher quality of inpatient EOL care, not just higher QOL of the patients as seen in the previous report [4]. Specifically, we have shown that advanced cancer patients with in-advance EOL discussions, as compared to those without EOL discussions, were more likely to have their inpatient HCPs inform and promote shared decision-making, encourage advance care planning, focus on individual, attend to the emotional and spiritual needs of the family, provide coordination of care, and support self-efficacy of their PCGs preparing for their dying and EOL care. One could hypothesize that if EOL discussions took place in advance, patients could start the process of preparing for their own EOL before they become seriously ill, and therefore could come up with their own specific needs, goals, wishes, and preferences regarding EOL care over time. This could make it significantly easier for an inpatient multidisciplinary team to match treatment with their unique perspectives.
This study has also demonstrated that up to 58 % of advanced cancer patients did not have EOL discussions with their primary oncologists or PCPs as of an average of 9 days prior to death, even though up to 80 % of them had metastatic disease. This discrepancy underscores the difficulties of having EOL discussions and transition to EOL care in a regular oncology clinic. Although emerging evidence suggests that in-advance EOL discussions and early palliative care involvement have a number of cascading benefits for advanced cancer patients and their family members [4, 15], conversations regarding prognosis, likely outcomes from available interventions, and alternatives or complementary interventions to disease-directed therapy occur too often very late in the disease trajectory or not at all [16]. Acknowledging this reality, the American Society of Clinical Oncology (ASCO) has recently published a special statement that emphasized the goals, barriers, and strategies of achieving individualized care for patients with advanced cancer [14]. The statement proposed that individualized cancer care should be delivered throughout the continuum of care, not just for patients at the terminal stage of life [14]. ASCO has also released a well-designed, user-friendly brochure outlining practical aspects of advanced cancer care planning from patients’ and families’ viewpoint [17]. This booklet not only discussed care options in advanced cancer and roles of the family in making treatment decisions but also provided advice on how to cope and find support at EOL with arranging one’s affairs, reviewing one’s life and religion/spirituality. With these efforts to increase education and awareness, it is hoped that individualized care toward EOL that match with our patient’s goals and preference will be achieved for advanced cancer patients regardless of their background.
This pilot study has limitations. First, an introduction of bias related to the surrogate nature and retrospective data collection is inevitable. This is especially true for the present study where PCGs of decedents who did not have EOL discussions were potentially more likely to suffer from psychological trauma as suggested by prior observation [4]. Second, the small sample size from a single institution may limit generalizability of the findings. Although the relatively low response rate could be a potential source of bias, previous survey studies among bereaved family members have commonly suffered from low response rates ranging from 21 to 70 % [3, 6–8, 18]. Third, we did not set an upper limit of an interview period. This may have resulted in the long time period between death and interview (mean duration 307.2 days) which could increase the threat of recall bias. The PCGs might not have been able to recall whether or not an EOL discussion occurred and whether it specifically occurred prior to the terminal admission. Fourth, the term “EOL discussions” could be interpreted differently by patients, PCGs, and physicians, reflecting the lack of its definition in the literature [19]. Nonetheless, we believe that our question to the study participants about in-advance EOL discussions addressed main issues related to EOL cancer care, since we applied the previously used question about such discussions [4] and specified three major elements (code status, living will, and medical power of attorney) that form the basis of most EOL discussions. Fifth, while we detected that patients without EOL discussions were significantly older than those with EOL discussions, we did not investigate detailed socioeconomic differences between those with and without such discussions. Future studies should address comprehensive patient-, PCG-, and HCP-related factors associated with the occurrence of in-advance EOL discussions. Lastly, we did not collect information about the person who initiated an EOL discussion (patient or family vs. HCP), though this could have unique implications. Most of these weaknesses were inevitable in this small, retrospective, after-death survey study. Our findings need to be investigated in prospective, larger studies.
Despite these limitations, our findings have some important clinical implications. First, the initiation of EOL discussions by primary oncologists and/or PCPs in clinic before an advanced cancer patient’s condition deteriorates may contribute to improving the quality of inpatient EOL care should they require a terminal admission to a hospital. Second, inpatient clinicians should identify seriously ill advanced cancer patients who have not had EOL discussions with their treating physicians. Since these patients are at high risk for receiving less optimal inpatient EOL care, an inpatient team needs to make an every effort to maximize palliative care resources. Third, advanced cancer patients, caregivers, and inpatient team should be reassured that high-quality EOL care can be delivered regardless of a code status on admission. Further investigations with larger prospective studies should be conducted to investigate (1) whether there is a cause–effect relationship between EOL discussions and the quality of inpatient EOL care, (2) how early EOL discussions have to occur, (3) how and with whom such discussions should be engaged, and (4) what aspects of EOL discussions contribute the most to quality EOL care
References
Nilsson ME, Maciejewski PK, Zhang B et al (2009) Mental health, treatment preferences, advance care planning, location, and quality of death in advanced cancer patients with dependent children. Cancer 115:399–409
Teno JM, Clarridge B, Casey V, Edgman-Levitan S, Fowler J (2001) Validation of Toolkit After-Death Bereaved Family Member Interview. J Pain Symptom Manage 22:752–758
Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, Mor V (2004) Family perspectives on end-of-life care at the last place of care. JAMA 291:88–93
Wright AA, Zhang B, Ray A et al (2008) Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300:1665–1673
Levin TT, Li Y, Weiner JS, Lewis F, Bartell A, Piercy J, Kissane DW (2008) How do-not-resuscitate orders are utilized in cancer patients: timing relative to death and communication-training implications. Palliat Support Care 6:341–348
Miyashita M, Morita T, Sato K, Hirai K, Shima Y, Uchitomi Y (2008) Good death inventory: a measure for evaluating good death from the bereaved family member’s perspective. J Pain Symptom Manage 35:486–498
Morita T, Hirai K, Sakaguchi Y, Maeyama E, Tsuneto S, Shima Y (2004) Measuring the quality of structure and process in end-of-life care from the bereaved family perspective. J Pain Symptom Manage 27:492–501
Miyashita M, Morita T, Hirai K (2008) Evaluation of end-of-life cancer care from the perspective of bereaved family members: the Japanese experience. J Clin Oncol 26:3845–3852
Connor SR, Teno J, Spence C, Smith N (2005) Family evaluation of hospice care: results from voluntary submission of data via website. J Pain Symptom Manage 30:9–17
Takesaka J, Crowley R, Casarett D (2004) What is the risk of distress in palliative care survey research? J Pain Symptom Manage 28:593–598
Mack JW, Weeks JC, Wright AA, Block SD, Prigerson HG (2010) End-of-life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol 28:1203–1208
Jackson VA, Mack J, Matsuyama R et al (2008) A qualitative study of oncologists’ approaches to end-of-life care. J Palliat Med 11:893–906
von Gunten CF (2008) Oncologists and end-of-life care. J Palliat Med 11:813
Peppercorn JM, Smith TJ, Helft PR et al (2011) American Society of Clinical Oncology statement: toward individualized care for patients with advanced cancer. J Clin Oncol 29:755–760
Temel JS, Greer JA, Muzikansky A et al (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. New Engl J Med 363:733–742
Keating NL, Landrum MB, Rogers SO Jr et al (2010) Physician factors associated with discussions about end-of-life care. Cancer 116:998–1006
American Society of Clinical Oncology. Cancer.Net (2011) Advanced Cancer Care Planning. http://www.cancer.net/patient/Coping/Advanced+Cancer+Care+Planning Accessed 22 February 2012
Shin DW, Choi JE, Kim JH et al (2011) What is the best practical survey method for the comparative assessment of palliative care services: results from a national quality assessment project in Korea. J Pain Symptom Manage 42:251–264
Hui D, Mori M, Parson HA, Kim SH, Li Z, Damani S, Bruera E (2011) The lack of standard definitions in the supportive and palliative oncology literature. J Pain Symptom Manage 43:582–592
Acknowledgments
We express our special appreciation to the Victoria Buffum Endowment Fund for its generous financial support and Vermont Cancer Center for its administrative support.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mori, M., Ellison, D., Ashikaga, T. et al. In-advance end-of-life discussions and the quality of inpatient end-of-life care: a pilot study in bereaved primary caregivers of advanced cancer patients. Support Care Cancer 21, 629–636 (2013). https://doi.org/10.1007/s00520-012-1581-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-012-1581-x