Abstract
Goals of work
To analyze cancer patient-related consultations of a telephone helpdesk (TH) for palliative care over a period of 5 years in the region of Utrecht, The Netherlands.
Materials and methods
A descriptive analysis was performed of consultations over a period of 5 years (2001–2006). The discipline and location of requesting professionals, patient characteristics, reasons for calling, symptoms, palliative care problems and needs for support were registered.
Main results
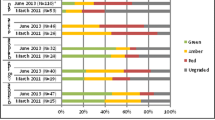
A total of 1,794 consultations were analyzed. There was an increasing number of consultations during the study period. Of the patients, 51% were male and their median age was 65 years (range 0–104). Eighty-four percent were treated at home by their general practitioner. Two thirds of the patients had a life expectancy <4 weeks. Most questions referred to pain (49%), delirium (20%), nausea and vomiting (16%) and dyspnea (12%). The median number of symptoms was 1 (0–6). Of the questions, 54% were related to pharmacological problems, 19% to psychological problems and 21% to the organization of care. Of the requesting professionals, 17% asked for support for themselves. Of the consultations, 14% were related to end-of-life issues: palliative sedation (11%) and euthanasia (3%).
Conclusion
After more than 5 years, the 24-h telephone consultation service fulfills a need for general practitioners dealing with daily dilemmas in palliative care treatment for cancer patients at home during the last period of their life.
Similar content being viewed by others
References
Ahmed N, Bestall JC, Ahmedzai SH, Payne SA, Clark D, Noble B (2004) Systematic review of the problems and issues of accessing specialist palliative care by patients, carers and health and social care professionals. Palliat Med 18:525–542
Barclay S, Wyatt P, Shore S, Finlay I, Grande G, Todd C (2003) Caring for the dying: how well prepared are general practitioners? A questionnaire study in Wales. Palliat Med 17:27–39
Bosanquet N, Salisbury C (1999) Providing a palliative care service: towards an evidence base. Oxford University Press, New York
Campbell C, Harper A, Elliker M (2005) Introducing ‘Palcall’: an innovative out-of-hours telephone service led by hospice nurses. Int J Palliat Nurs 11:586–590
De Graeff A, Verhagen EH, Eliel MR, Hesselmann GM, Kroeze-Hoogendoorn (eds) (2002) Richtlijnen palliatieve zorg (guidelines for palliative care). Comprehensive Care Centre Middle Netherlands, Utrecht
Groot MM, Vernooij-Dassen MJ, Courtens AM et al (2005) Requests from professional care providers for consultation with palliative care consultation teams. Support Care Cancer 13:920–928
Hearn J, Higginson IJ (1998) Do specialist palliative care teams improve outcomes for cancer patients? A systematic literature review. Palliat Med 12:317–332
Higginson I (1999) Palliative are services in the community: what do family doctors want? J Palliat Care 15:21–25
Homsi J, Walsh D, Nelson KA et al (2002) The impact of a palliative care consultation service in medical oncology. Support Care Cancer 10:337–342
Jansen-van der Weide MC, Onwuteaka-Philipsen BD, van der Wal G (2006) Quality of consultation and the project ‘Support and Consultation on Euthanasia in the Netherlands’ (SCEN). Health Policy (in press)
Kendall C, Jeffrey D (2003) Out-of-hours specialist palliative care provision in an oncology centre: is it worthwhile? Palliat Med 17:461–464
Kuin A, Courtens AM, Deliens L, Vernooij-Dassen MJ, van Zuylen L, van der Linden B, van der Wal G (2004) Palliative care consultation in the Netherlands: a nationwide evaluation study. J Pain Symptom Manage 27:53–60
van der Linden B, Jansen G, Meijers B (2000) Helpdesk Palliatieteam Midden Nederland: resultaten van het eerste jaar (Helpdesk Palliative Care Team Middle Netherlands: results of the first year). University of Utrecht, Utrecht
Rabow MW, Dibble SL, Pantilat SZ, McPhee SJ (2004) The comprehensive care team: a controlled trial of outpatient palliative medicine consultation. Arch Intern Med 164:83–91
Rietjens JA, van der Heide A, Vrakking AM, Onwuteaka-Philipsen BD, van der Maas PJ, van der Wal G (2004) Physician reports of terminal sedation without hydration or nutrition for patients near death in the Netherlands. Ann Intern Med 141:178–185
Rinck GC, van den Bosch GAM, Kleijnen J et al (1997) Methodological issues in the effectiveness research on palliative cancer care: a systematic review. J Clin Oncol 15:17–27
Royal Dutch Medical Society (2005) Guideline on palliative sedation. Utrecht, The Netherlands
Schrijnemaekers V, Courtens A, Kuin A et al (2005) A comparison between telephone and bedside consultations by palliative care consultation teams in the Netherlands: results from a nationwide registration. J Pain Symptom Manage 29:552–558
Schuit KW, Bender W, Meijler WJ, Otter R, Meijboom-De Jong B, Sleijfer DT (1999) Learning effects of a workshop in palliative cancer care for general practitioners. J Cancer Educ 14:18–22
Schuit KW, Otter R, Stewart R, Sleijfer DT, Meijler WJ, Meijboom-De Jong B (2000) The effects of a postgraduate course on opioid-prescribing patterns of general practitioners. J Cancer Educ 15:214–217
Acknowledgements
The development of the palliative care service Utrecht as part of the Center for Development of Palliative Care Middle Netherlands was funded by the Dutch Ministry of Health, the Comprehensive Cancer Center Middle Netherlands and the University Medical Center Utrecht.
We are grateful to the partners in the nationwide Program for Development of Palliative Care and to Professor Guus Schrijvers for his support in the first evaluation of concepts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teunissen, S.C.C.M., Verhagen, E.H., Brink, M. et al. Telephone consultation in palliative care for cancer patients: 5 years of experience in The Netherlands. Support Care Cancer 15, 577–582 (2007). https://doi.org/10.1007/s00520-006-0202-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-006-0202-y